
Why Ice Isn’t Nice: The Surprising Truth About Using Ice for Injuries?

If you’ve ever tweaked a joint or muscle in your life, you’re well acquainted with the trusty ice pack.
Have you ever examined the truth behind ice for injuries, swelling, and pain? In this article, I'm going to review the science and research for using ice on injuries to help you heal faster.
I’m not here to bash ice packs and cold therapy. Instead, I hope to bring you the science and evidence to cut through the misinformation available. You will better handle your injuries, aches and pains without wasting time or money. In fact, I still occasionally uses ice for my patients (just not for myself). Much like my patients, I will provide you with information and you can make your own unbiased decision.
Ice makes intuitive sense but isn't used as intended
Here’s the logic:
Ice vasoconstricts blood vessels. This means it will shrink the diameter of vessels (think arteries and veins). Logically, if we place ice on the area that’s swelling it will constrict the vessels and reduce swelling right? Here’s where we S&T (stop and think).
"Why would you want to reduce the availability of a product that has evolved over hundreds of thousands of years?"
Your mind is ingrained with the idea that "Inflammation is bad". You don't even consider the benefit that it brings. Your body is a well-oiled machine with mechanisms that have developed to protect, repair, and strengthen itself. If, and only if, you get out of the way. Your goals after an injury are to protect, recover/restore, and minimize muscle loss.
- REAL LIFE vs RESEARCH:
Studies: Research that shows effective changes to blood flow use ice that is colder than a polar bear’s toenail for an extended period of time.
Real Life: In real life, people apply a moderately cold ice pack over 2 layers of clothing or wrapped by a towel. The only constricting this is doing is in your clothes!
Before moving on, let’s review the process by which your body handles inflammation after an injury and how ice would fit into the equation.
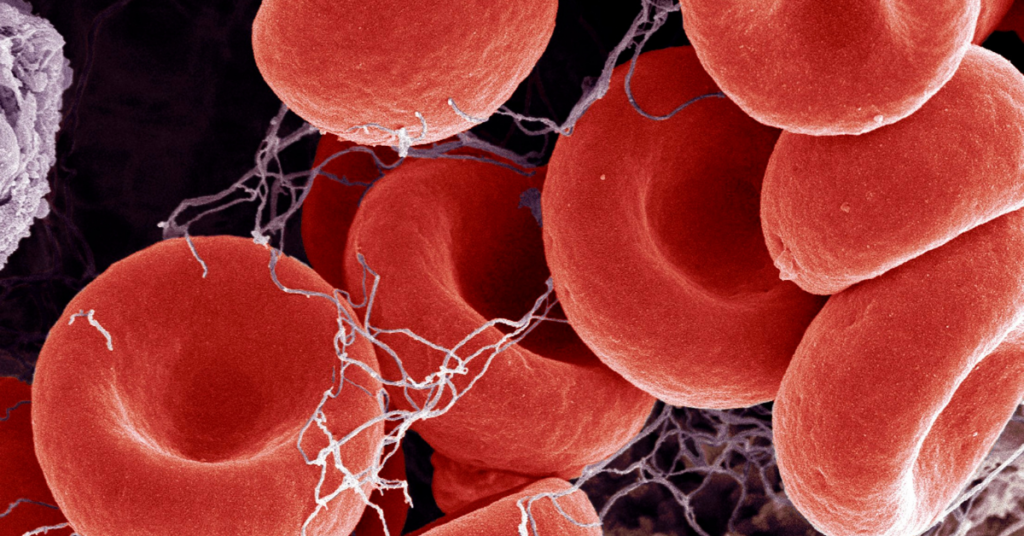
The lymphatic system removes swelling from an injured site. Your lymphatic system DOES NOT have a heart working around the clock like your circulatory system. Instead, it’s a passive system that relies on your muscle’s contraction as the engine. The muscle contraction pumps to rid your body of excess fluid.
Again, inflammation happens for a reason. Dr Bahram Jam has a great analogy:
“If you cut yourself, would you take
an anti-coagulant (blood thinner) to stop the clotting process?
Of course not! It’s a tremendous system!”
So why would you want to stop or slow down the inflammatory process after an injury?
The use of ice lacks significant evidence from meaningful randomized control trials.
A handful of studies actually show value and the chance of harm. However, they are not quality, randomized controlled trials. If a study is not a randomized control trial, it’s of little to no value.
A randomized control trial removes bias and has a verified outcome. Both of which are critical to effective science. Otherwise they are using reports of symptoms which opens the door to bias.
A 2006 Cochrane review on low back pain...
CONCLUSION - There is some evidence supporting the use of heat but no evidence on the use of cryotherapy (ice).
A 2012 analysis looked at 11 trials involving 868 patients...
CONCLUSION - There is insufficient evidence to determine the relative effectiveness of RICE (rest, ice, compression, and elevation) therapy for acute ankle sprains. (Vandenbockrom citation)
Think of our body like a highway with an accident somewhere along the line. Would you want to shrink the highway from 4 lanes to 2 just when the emergency and clean-up crew is on the way? Of course not!
If you cut yourself, would you consider doing something to stop or slow the clotting process? Of course not!
The issue that most people want to avoid is actually persistent swelling.
Persistent swelling becomes an issue not because of the clean-up crew coming to the scene. Congestion makes it impossible for the clean up crew to leave after it's complete. It’s like that accident happened on the busiest highway near your home. It can take hours to clear due to the amount of congestion!
Icing would be like slowing the influx of additional cars coming into the highway. This may help lessen additional build up. But in no way will ice help the congestion that is already at the accident scene (aka actual healing). This is due to the fact that you would actually be shrinking (vasoconstricting) the exit ramps. In turn, this may actually worsen the congestion!
The answer is to focus on 3 things:
- Decongestion (clearing the area)
- Safety (protecting the injured tissue)
- Loss prevention (minimizing atrophy of surrounding muscles)
This will let the body do what it does best - signal and call for appropriate healing activity.
Now, if I’m starting to make some sense, but your hesitant to buy, pick up a dual-purpose hot/cold pack. You can pop them in the microwave to use as a hot pack for low back pain, but can leave it in the freezer in case you still have that urge to ice (keep reading to see when ice is actually useful). Click on the link for my recommended dual-purpose pack. It’s an amazon affiliate link so if you’re looking for one anyway, please click on the link. I get a small commission from Amazon which helps me continue with this site and channel.
Powered Low Back Hot pack with strap
https://amzn.to/34kbgyv
Microwavable Hot/Cold Pack
https://amzn.to/30maKic
NEXT SIMILARITY:
3 . They both give us a feeling of control.
As humans, there is nothing we dread more than feeling helpless. There are some times where intervening is helpful and in fact essential (you suffer a compound fracture and your bone is poking out through your skin-Yikes!). Other times, it’s preferable to let your body do what it does best.
In coaching youth sports, I rarely see a player suffer an injury without a parent or coach feeling like they need to intervene with an ice pack. Placebo can certainly play a factor here. That’s not a bad thing. Humans balance risk. There’s something called risk homeostasis. If you're protected from one thing, you lower your guard on others. This leads to unintended consequences
You spend all night standing with my friends with a newly sprained ankle because you can “ice it later".
Here are 3 scenarios where ice would classically be applied. I'll explain the science and research, and talk about what you should actually do in each scenario.
SCENARIO 1 - Inflammation in a New Injury
Your kid falls and bumps their elbow , you sprain your ankle, you or a loved one has surgery.
- Studies have shown that ice may be beneficial IMMEDIATELY after the injury by potentially reducing injury to surrounding tissue by limiting inflammatory mediators into healthy, accessory tissue spaces.
- We’ll discuss ice for pain in a later scenario
BEWARE – Often times, the acute pain is simply because of congestion. Icing doesn’t help the congestion. It doesn’t even make sense that it would!
Research following total knee replacement (TKA) concluded that cryotherapy (ice) after surgery resulted in small improvements in ROM but provided no benefits on pain, pain medication use, swelling or functional outcomes (Adie et al 2010, 2012).
Clinical trials on the efficacy of RICE (Rest, Ice, Compression, Elevation) have supported the use of compression but have found no value in icing (other than a temporary numbing effect) (Hubbard et al 2004).
Does the body really need help in reducing inflammation? The lymphatic system naturally and slowly removes all the waste products and excess fluid buildup caused by the inflammatory process. Elevation and compression may assist the lymphatic system in its efforts at draining excess fluid but the impact is likely minimal. Interestingly, studies have shown that icing may actually reduce skeletal muscle contraction (Bleakely et al 2012). This could result in a temporary reduction in lymphatic drainage at the injury site.
Perhaps most significant, was a 2012 paper published in the Journal of Athletic Training. The author’s concluded that
“The practice of using ice to treat sprained ankles is based largely on anecdotal evidence. Evidence to support the use of ice in the treatment of acute ankle sprains is limited.” – Journal of Athletic Training 2012
“The practice of using ice to treat sprained ankles is based largely on anecdotal evidence. Evidence to support the use of ice in the treatment of acute ankle sprains is limited.”
Journal of Athletic Training 2012
RECOMMENDATION – track your loading vs unloading schedule daily and manipulate the amount of time you spend on your feet. When you are not standing, use elevation and compression to assist in drainage. Actively contracting the nearby muscles to assist in fluid return is paramount. Ice can be used, but for pain relief only.
SCENARIO 2 - Persistent Swelling
If you’re suffering from chronic systemic (or body wide) inflammation, this is entirely different. What I’m referring to is a localized area of chronic pain. A classic example would be arthritis. If you’re knee is swollen all the time, you must address the underlying movement issues that are leading to the arthritis in the first place. As for the inflammation, the focus should be on regular decongestion as discussed in the previously. One way we help this in our PT centers is through the use of muscle pumping electric stimulation devices. This is an Affiliate link for a MarcPro unit that is similar to what we use in our physical therapy centers. It produces a muscle contraction resulting in a pumping like removal of the inflammation.
MarcPro
Marc Pro Plus
SCENARIO 3 - Soreness after a workout
There is a notion that using ice after a workout will reduce the degree of muscle soreness that you will experience in the following days.
A 2013 study by Tseng et al examined this very notion about ice. Does icing muscles after a hard athletic workout help recovery and promote earlier return to activity?
Interestingly, their findings demonstrated the opposite to occur. After performing 6 sets of a heavy triceps workout, half the athletes were randomly placed into groups that received either 15 minutes of cooling ice pack or a sham ice pack. After 2 and 3 days the ice group had significantly greater creatine kinase and myoglobin (which are signs of muscle overload). They also reported having more triceps fatigue than the sham ice group.
“These data suggest that topical cooling, a commonly used clinical intervention, seems to not improve but rather delay recovery from eccentric exercise-induced muscle damage”.
It gets worse. A 2019 study by Earp et al found that icing (with cold water immersion) after resistance exercise significantly reduced testosterone after exercise. This supports prior studies that have shown a reduction in muscle protein synthesis after resistance training when ice baths are added.
The purpose of doing any type of resistance work is to gain strength which relies on your body’s ability to synthesize protein. Adding ice potentially thwarts this effort by reducing testosterone and new protein growth? Sounds like a great idea!
SCENARIO 4 - Pain
This is conclusive! Ice slows all metabolic activity including firing of nociceptors or pain nerves. Translation: ICE HELPS PAIN…..temporarily.
A 2004 Systematic Review from Hubbard concludes that cryotherapy seems to be effective in temporarily reducing pain and providing a localized numbing effect.
Studies looking at ice after ACL surgery find that icing added no additional benefit with respect to reducing swelling or improving ROM. Ice does significantly lower post-op pain and potentially reduced the use of pain meds (Raynor et al 2005).
ORIGIN STORY
Perhaps most importantly, Dr Gabe Mirkin, the physician that coined the term RICE no longer promotes it. I quote - “It’s perfectly fine to ice if you want, but realize it’s delaying healing,” Dr. Mirkin said, “[Icing] is not going to change anything in the long term.”
Instead of icing to reduce inflammation, athletes might be better off letting it run its course. Better yet, get moving again, Mirkin said: “Don’t increase your pain, but you want to move as soon as you can.” This isn’t to say ice has no physiological effect. Since we know that ice helps reduce pain, it can cut down on pain medication use and allow you to get things moving sooner.
“It’s perfectly fine to ice if you want, but realize it’s delaying healing. Icing is not going to change anything in the long term.”
- Gabe Mirkin, MD
If I've sparked an interest and you'd like to learn more, check out Gary Reinl's book ICED.
Book - "ICED" by Gary Reinl
https://amzn.to/36D48jD
There's always new research on the horizon. It’s safe to say, if you're trying to help your injury and inflammation, its best to leave the ice where it works best.

There’s something to be said for GENUINELY believing that something is helping you. The Placebo effect is real and has a tremendous impact. If you’re someone that feels ice is critical to your recovery, have at it!
But if you’re like most people, and actually dislike that frozen feeling, you can safely place that ice pack down and keep it moving!
Remember, next time you have an injury, it's likely related to how you control your movement. If you're not back to feeling your best, it's a must that you find a movement specialist to help get you back on track.
Join the Movement by Subscribing to my YouTube channel - MovementprojectPT
https://www.youtube.com/c/movementprojectpt?sub_confirmation=1
Sign up for the newsletter


